As research subjects viewed emotion-laden pictures while an fMRI (functional magnetic resonance imagining) machine scanned their brains for activity, researchers in a Cornell-University of British Columbia-University of Toronto study began to think: Perhaps our genes really can regulate response to emotional information.
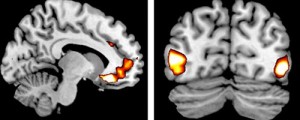
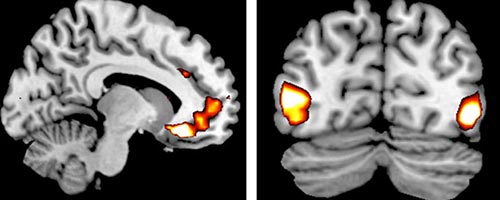
Carriers of a genetic variation (the ADRA2b deletion variant) showed more vivid perceptions of emotional events (called emotionally enhanced vividness or EEV), which was associated with more activity in a region of the brain responsible for regulating emotions and evaluating pleasure and threat (the ventromedial prefrontal cortex), researchers reported in the April 22 Journal of Neuroscience.
The 2014 study was a relatively small one, with 39 subjects undergoing fMRI scans at the University of Toronto. Slightly more than half (21) carried the ADRA2b deletion variant, and the rest did not. But the result was clear. Some people are genetically wired, as the researchers report, to “enhance the subjective vividness of perceptual experience and its emotional enhancement.”
“Emotions are not only about how we feel about the world, but how our brains construct our perception of it,” says Adam K. Anderson, Cornell associate professor of human development and the study’s senior author.
“Our genes influence how our brains see the positive and negative aspects of our world more vividly. As a result, we may come to mistakenly believe the world has more rewards or threats.” “People really do see the world differently,” said Rebecca Todd, first author and assistant professor of psychology at the University of British Columbia. “For people with this gene variation, the emotionally relevant things in the world stand out much more.”
Todd said she believes emotionally enhanced vividness may help explain why some people are more susceptible to PTSD (post-traumatic stress disorder) and intrusive memories following trauma.
The report is titled “Neurogenic Variations in Norepinephrine Availability Enhance Perceptual Vividness.” The study was supported, in part, by the Canadian Institutes of Health Research.